Chronic Unease In Resuscitation
Billy Doyle Lead Instructor Resuscitation Skills
"Chronic unease refers to the experience of discomfort and concern about the management of risks. It is a healthy scepticism about one's own decisions and the risks that are inherent in work environments."
The concept of Chronic Unease was originally developed by the oil and gas industry (Royal Dutch Shell Oil) as a feature of working towards the goal of zero harm within their industry. When things go wrong on a oil drilling rig it goes spectacularly wrong and results in catastrophic harm including massive loss of life, environmental damage and financial loss.
It is proposed that as an organisation, being in a constant state of unease at every level of human interface from the worker on the front-line to senior management and executives critically supports their safety record.
Chronic Unease is a mind set that fosters a healthy world view that:
- ''Even though I do not expect something to be wrong, I am constantly on guard and prepared for when it does go wrong."
- "I am constantly looking for weak signals that maybe an early indication that there is a hole in the system and this event no matter how minor could lead onto greater failure so I will act now."
- "I will question assumptions and withhold jumping to conclusion"
What can we learn from the concept and attributes of Chronic Unease in resuscitation?
Let's look at the components that engender a state of Chronic Unease and draw some parallels to managing a clinical team in a high stakes medical scenario.
Imagine a 55 year old male presents to your accident and medical clinic. He looks unwell. He is short of breath and complaining of chest discomfort. He is triaged as urgent and wheeled into resus. Your small team of one nurse and another medical colleague goes to work, an ambulance is called as is the cardiology registrar at your local hospital and yes it looks like this gentleman is suffering an acute coronary syndrome with elevated ST segments in lead II,III,AVF and V1 & V2. He is struggling. Looks ashen and something deep inside screams : "Uh-oh."
Just another STEMI? Fingers crossed he makes it to hospital?
I'm not going to run through the clinical management of this situation, rather view this situation wearing a cloak of Chronic Unease to see what thought processes and actions might augment how we manage human and clinical resources in order to be prepared if this patient 'circling the drain' suddenly suffers a cardiac arrest.
Attributes of Chronic Unease
The ability to mentally project the development of a situation into the future based on its current state.
The thinking here is to use sound clinical judgments based on good evidence on the potential clinical picture that may develop. Get real. Sure, everyone has the potential to suffer cardiac arrest, but there are prodromes that stratify some more likely than others. When that signal is present, acknowledge it, even declare it to the team so they share your mental model of the situation and share your unease. Activate help early, (even if it is eventually not required). If a crises develops you do not want to be behind eight-ball.
In this clinical situation a clinician adopting safety imagination might preemptively place defibrillation pads, they might clear the bed space of clutter, they might pull the team aside and pre allocate roles and tasks that maybe required. The bag-mask resuscitator might be pulled out from the draw and assembled. The suction made ready. All "just in case."
A personality trait reflecting a tendency to resist complacency and to anticipate failure.
Are you some one who with a little voice in their head that runs scripts like: "No... can't be that bad, he'll be fine,everything is O.K...," despite compelling evidence to the contrary? There are a number of scripts that can run contrary to the reality of any given situation and these are complex cognitive errors beyond the scope of this article. Suffice to say, a personality trait that resists the urge to dismiss weak signals when events are unravelling takes discipline and practice. It needs to be a habit.
Is there anything wrong with being pessimistic, resisting the urge to be complacent and therefore taking steps to anticipate failure? Its all about context. If you've developed the habit of pessimism, this trait runs subconsciously in the background of thought and becomes dominant when you're receiving weak signals that something is wrong.
A clinician may also take a healthy dose of pessimism when planning resuscitation skills. Sure, we all like to think we can perform advanced airway skills like endotracheal intubation and high-quality CPR. The answers to pessimistic questions might scale back you're immediate expectations of what you think you should do to a more realistic position of what you can do in reality. Pessimistic questions might include:
"But when was the last time I did that, do I have skilled help to assist, do I have the right equipment, there are only two of us here. How long could we realistically do effective chest compressions?"
The ability to notice and identify (weak) signals of risks in the environment.
In the context of the oil and gas industry, this may mean paying attention to hazards such as liquid spilled on the bottom of a stairwell or a pressure alarm that is intermittently going off for some unexplained reason.
In our clinical situation the weak signals may be subtle. A 1 or 2% drop in oxygen situations. A 5 mmHg drop in systolic blood pressure. The patient might be fidgeting and constantly fiddling with their nasal prongs where as previously the seemed settled, possibly indicating a subtle change in their level of consciousness. Over all not drastic changes, no single signal means much, but combined may signal something more sinister. Combined with safety imagination (remember these judgments are based on good evidence) weak signals like these should trigger further unease and prompt action to avert or plan for crises if possible.
A tendency to worry about risk and safety.
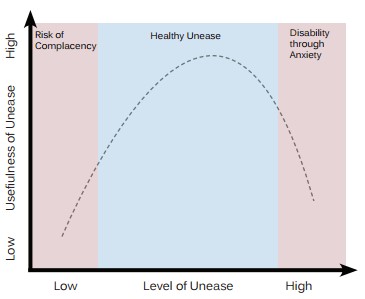
Lets be clear. The workplace is no fun if everyone is worried all the time and in the extreme, worry can produce pathology. A tendency to worry is however the counter balance to complacency.
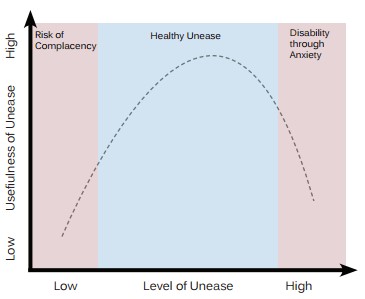
Dr. Lauren Fruhen: Chronic Unease: A state of Mind for Managing Safety. Centre for Safety. The University of Western Australia
Whether you have been involved in an incident before.
It is true clinicians can have thought biassed towards the frequency of past events. If a new event presents similar to one encountered previously clinicians can be drawn to favour a clinical diagnosis based on the previous like case.
The same goes for crises. It is human nature to over react to a situation if a previous event like the one encountered didn't go well or had less favourable outcomes. Reflecting on previous crises and the lessons learnt can strengthen performance in the future. Experience of similar adverse events in the past gives the clinician a 'heads-up' to the present and might shape an accurate mental model of the situation that others may not share as they may not have read the signals of an unfolding crises.
At the same time, other members of the team may have experienced an adverse event more recently than the lead clinician and they have a 'heads-up'. A flattened hierarchy is encouraged so team members, no matter their position in the hierarchy or profession are encouraged to speak up: "The last time I saw a patient like this he suffered a cardiac arrest" maybe all it takes for a team member to jolt a team out of complacency into a state of chronic unease.
Ability to question assumptions and not jumping to conclusions.
Thinking is complex. Explaining thinking even more-so. If we accept the reality that human thinking can be flawed, that we will and do err with alarmingly frequency, then that mindfulness will serve us well when analysing thought through the lens of Chronic Unease.
Crises and high stakes situations rob us of the time required for slow powerful thought so there is a tendency to revert to rule-based thinking during a crises. Rightly or wrongly, this default thinking can expedite a solution (if the right rule is applied for the right situation). An individual with a habit of Chronic Unease accepts there are occasional failings in their own and the team's reasoning and the rules used to solve problems. They remain open to the possibility of other solutions and encourage input from others. Because they have accepted these human factors they use cognitive aids such as algorithms and check-lists to guide problem solving and formulating a management plan.
In our clinical case, examples of where a state of Chronic Unease shapes behaviour might include accessing cardiac arrest algorithms and quickly reviewing the first few steps (just in case). It might include ignoring an underlying assumption that the ambulance will only be five minutes away because it always is. Continually questioning the clinical evidence you perceive matches your assumed clinical diagnosis and cross-checking your thinking with others. Seeking expert help early and constantly avoiding the temptation of jumping to the conclusion when the patient shows signs of improvement with a script like : "Everything Is O.K, everything will be O.K." is an attribute of Chronic Unease.
Summary
Chronic Unease is not a novel concept. It is used in many high stakes industries such as oil and gas and the aviation industry.
Resuscitation Skills includes and supports the inclusion of instruction in effective teamwork and communication in the Advanced Resuscitation Courses on offer. Its inclusion in such courses is long over due.
Perhaps the attributes of Chronic Unease offers some solutions for a healthy approach to pre-crisis phase of medical emergencies.
Very little, (if anything) is published on the attributes of Chronic Unease in medicine. It would be a fascinating investigation.
I welcome comments and thoughts.
[email protected]